
For most people, a generic pill works just like the brand-name version. But how does the FDA know it’s truly the same? You might think they test it on humans every time. They don’t. In many cases, they skip human trials entirely-and rely on a test tube instead.
What Is a Bioequivalence Waiver?
A bioequivalence waiver, or biowaiver, is when the FDA says: you don’t need to run a human study to prove your generic drug works like the original. Instead, you can use in vitro data-dissolution tests in lab conditions-to show the two products behave the same way in the body. This isn’t a loophole. It’s science. If a drug dissolves the same way in simulated stomach fluid, and it’s absorbed easily by the body, then it’s highly likely to perform the same in people. The FDA has spent decades validating this approach. For certain types of drugs, in vitro testing is more reliable than human trials.When Does the FDA Allow This?
The rules are strict, but clear. Biowaivers only apply to immediate-release solid oral dosage forms-think tablets or capsules you swallow, not liquids, injections, or slow-release pills. The key is the Biopharmaceutics Classification System (BCS). This system sorts drugs into four classes based on two things: how well they dissolve in water (solubility) and how well they cross into your bloodstream (permeability). - BCS Class I: High solubility, high permeability. These are the easiest to waive. Examples: metformin, atenolol, ranitidine. - BCS Class III: High solubility, low permeability. Possible, but harder. The drug must have identical ingredients and no site-specific absorption. Examples: acyclovir, cimetidine. For Class I drugs, the FDA requires:- Drug dissolves ≥ 85% within 30 minutes in pH 1.2, 4.5, and 6.8 buffers
- Dissolution profiles of test and reference products match with an f2 similarity factor of ≥ 50
- Drug substance is highly soluble (dose number ≤ 1 across pH 1-6.8)
- Drug is highly permeable (≥ 90% absorbed in humans)
Why Skip Human Studies?
Running a bioequivalence study in people costs between $250,000 and $500,000. It takes 6 to 12 months. You need healthy volunteers, blood draws, lab analysis, regulatory paperwork, and ethical reviews. For a generic company making 10 products a year, that’s $2.5 million to $5 million just in clinical costs. And that’s not counting delays. A single study can hold up an entire product launch. Biowaivers cut that down to a few weeks and a fraction of the cost. One generic manufacturer reported saving $4.2 million over three years by using biowaivers for 12 products. Each one shaved off 8-10 months from approval time. It’s not just about money. It’s about ethics. Why test 24 healthy people on a drug that’s already proven safe and predictable? If dissolution data can reliably predict performance, the FDA agrees: don’t subject people to unnecessary procedures.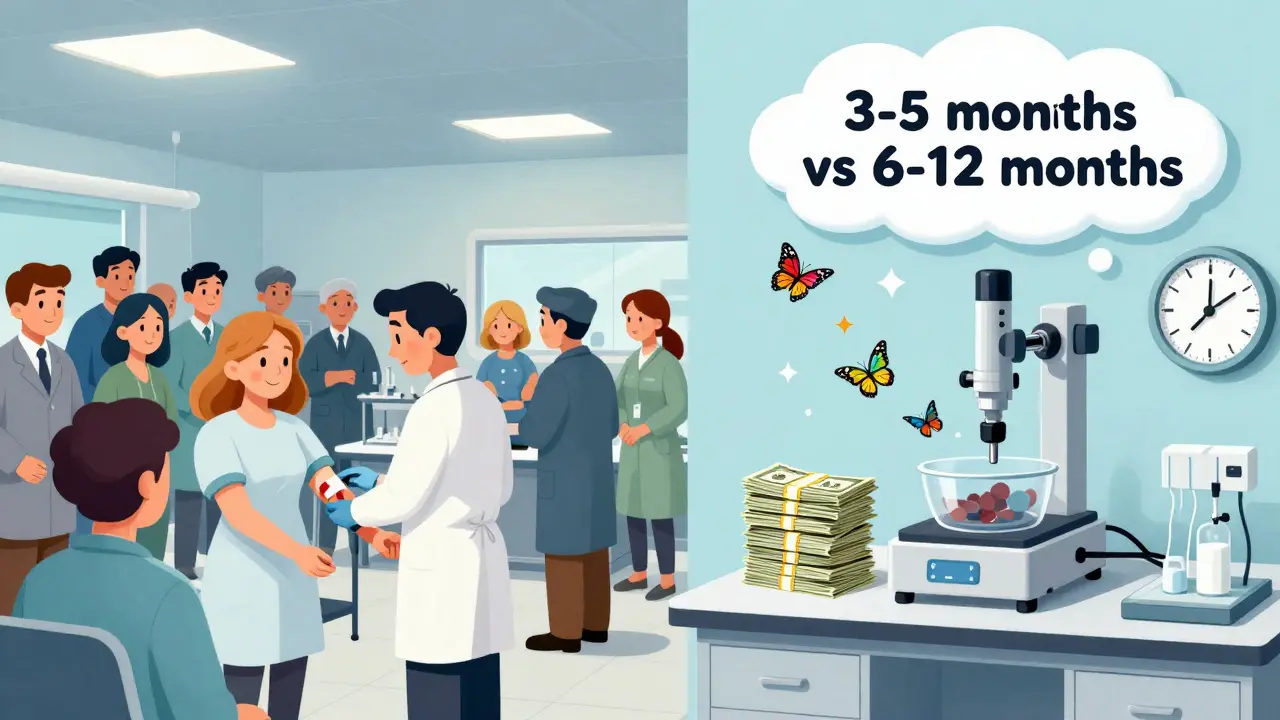
What Doesn’t Qualify?
Not all drugs get a pass. The FDA won’t waive in vivo studies for:- Modified-release products (extended-release, delayed-release)
- Narrow therapeutic index drugs (like warfarin, levothyroxine, digoxin)-except for a few antiepileptics with specific guidance
- Drugs with complex formulations (liposomes, nanoparticles, suspensions)
- BCS Class II or IV drugs (low solubility)
How to Get a Biowaiver Approved
It’s not just filling out a form. You need hard data and a clear story. 1. Classify your drug using published BCS data or your own solubility/permeability studies. 2. Develop a dissolution method that’s physiologically relevant and discriminatory. Test at least 12 units per batch. Sample at 10, 15, 20, 30, 45, and 60 minutes. 3. Compare dissolution profiles using the f2 similarity factor. If it’s below 50, you’re not approved. 4. Document excipient similarity down to the exact type and percentage. No guesswork. 5. Submit early. Companies that use the FDA’s Pre-ANDA meeting program have a 22% higher approval rate. The whole process takes 3-5 months for experienced teams. For newcomers, it can take longer. Many small companies skip biowaivers because they don’t have the in-house biopharmaceutics expertise.How Common Are Biowaivers?
In 2018, about 12% of ANDA submissions for solid oral drugs used biowaivers. By 2022, that jumped to 18%. That’s thousands of products approved without a single human subject. The FDA’s own data shows a 78% approval rate for complete submissions. That’s high-but only if you follow the rules. Incomplete data? Rejected. Poor dissolution method? Rejected. Wrong drug class? Rejected. Big players like Teva and Mylan use biowaivers in 25-30% of their pipelines. Smaller companies? Only 10-15%. Why? It takes resources: scientists who understand dissolution, regulatory writers who know the guidance, and time to validate methods.
What’s Changing?
The FDA isn’t standing still. In 2022, they released a draft guidance to expand biowaivers to more BCS Class III drugs. In 2023, they launched a pilot program to test waivers for certain narrow therapeutic index drugs. They’re also investing $15 million a year through GDUFA to improve in vitro-in vivo correlation models. Their 2023-2027 plan aims to expand biowaiver opportunities by 25%. But challenges remain. Eighty-five percent of complex generics-like patches, inhalers, or long-acting injectables-still can’t use biowaivers. The science isn’t there yet.Is This Safe?
Over 95% of BCS Class I biowaivers have matched up with actual human bioequivalence results, according to the American Association of Pharmaceutical Scientists. That’s better than many in vivo studies. Think of it this way: if you know a drug dissolves completely and gets absorbed quickly, and you’ve tested it under every stomach condition, you don’t need to give it to 24 people to prove it works. You’re not guessing-you’re measuring. The FDA doesn’t approve biowaivers lightly. They’ve spent decades validating this approach. They’ve reviewed hundreds of submissions. They’ve published detailed guidance. And they’ve seen the results.What’s Next?
Expect more biowaivers in the next few years. As methods improve and more drugs are classified, the list of eligible products will grow. The goal isn’t to cut corners-it’s to cut waste. Eliminate unnecessary human testing. Speed up access to affordable medicines. Keep the science strong. For generic manufacturers, it’s a lifeline. For patients, it means faster access to cheaper drugs. For regulators, it’s proof that smart science can replace outdated practices. The future of bioequivalence isn’t in blood samples. It’s in dissolution profiles. And the FDA already knows it.Can any generic drug get a bioequivalence waiver?
No. Only immediate-release solid oral dosage forms that meet BCS Class I or, in limited cases, Class III criteria qualify. Modified-release products, narrow therapeutic index drugs, and complex formulations are excluded. The drug must have high solubility and, for Class I, high permeability. Dissolution profiles must be nearly identical to the brand product.
How long does a biowaiver application take to get approved?
The review process for a biowaiver request is typically faster than a full in vivo study, but preparation takes time. A well-prepared submission with complete dissolution data and justification can be reviewed in 6-10 months. However, developing the dissolution method and validating it can take 3-5 months before submission. Companies that use FDA’s Pre-ANDA meetings often see faster approvals.
Why do some biowaiver requests get rejected?
The most common reason is inadequate dissolution method discrimination-meaning the test can’t reliably tell the difference between the generic and brand product. Other reasons include mismatched excipients, insufficient data on solubility or permeability, or failure to meet the f2 similarity factor of ≥50. About 35% of rejections in 2021 were due to poor method validation.
Do biowaivers apply to all countries?
Many countries follow the FDA’s lead. The International Council for Harmonisation (ICH) issued M9 guidance in 2021, which standardizes BCS-based biowaivers across the U.S., EU, Japan, and other members. While each region has slight variations, the core principles are aligned. Companies using FDA-approved biowaivers often leverage the same data for submissions abroad.
Is it cheaper to get a biowaiver than to run a human study?
Yes, dramatically. A single in vivo bioequivalence study costs $250,000-$500,000 and takes 6-12 months. A biowaiver submission costs $20,000-$80,000 in development and testing, and takes 3-6 months to prepare. For companies submitting multiple products, the savings run into millions annually. The FDA estimates biowaivers have accelerated generic approvals by an average of 7.3 months per product.






Jeffrey Frye
December 24, 2025 AT 01:09Delilah Rose
December 24, 2025 AT 03:26Lindsey Kidd
December 25, 2025 AT 04:09Rachel Cericola
December 26, 2025 AT 04:55CHETAN MANDLECHA
December 26, 2025 AT 05:15Ajay Sangani
December 28, 2025 AT 05:13Pankaj Chaudhary IPS
December 28, 2025 AT 18:41Aurora Daisy
December 30, 2025 AT 14:23Paula Villete
December 30, 2025 AT 18:00Georgia Brach
January 1, 2026 AT 09:00Katie Taylor
January 3, 2026 AT 03:02Payson Mattes
January 3, 2026 AT 21:14Isaac Bonillo Alcaina
January 4, 2026 AT 19:05Bhargav Patel
January 6, 2026 AT 09:06Steven Mayer
January 8, 2026 AT 01:26