Chronic Alcohol Use Disorder isn’t just about drinking too much. It’s a medical condition where your brain and body become so dependent on alcohol that stopping feels impossible-even when it’s destroying your health, relationships, or career. This isn’t weakness. It’s biology. Every time you drink, alcohol rewires your brain’s reward system. Over time, your body starts needing alcohol just to feel normal. That’s the core of Alcohol Use Disorder (AUD), and it affects more than 14 million adults in the U.S. alone.
What Happens to Your Body When You Drink Too Much for Too Long
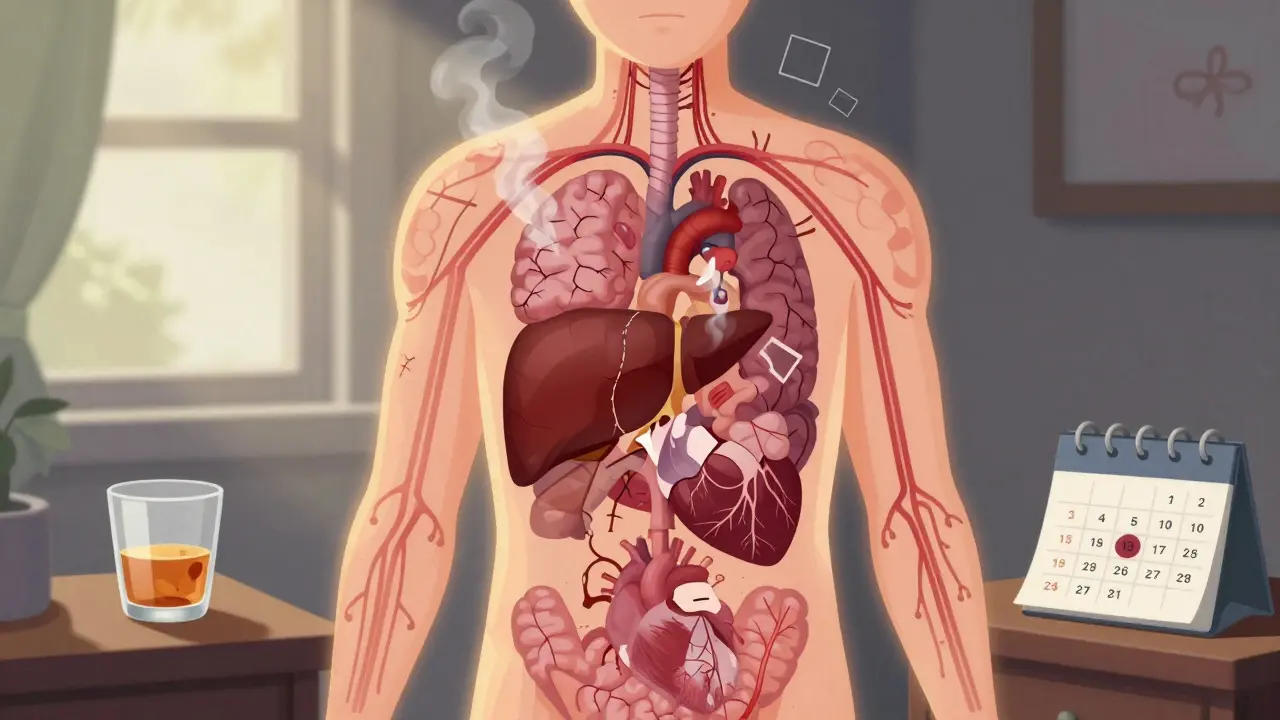
Alcohol doesn’t just hit your liver-it spreads through your bloodstream and touches nearly every organ. Early signs are easy to miss: needing more drinks to get the same effect, feeling anxious when you haven’t had a drink, or drinking to calm nerves. But over months or years, the damage builds silently.
Your liver takes the hardest hit. About 90% of heavy drinkers develop fatty liver disease first. It’s reversible-if you stop drinking. But if you keep going, inflammation kicks in. Alcoholic hepatitis follows, with symptoms like jaundice, fever, and belly pain. Left untreated, it leads to cirrhosis: scar tissue replacing healthy liver cells. Once cirrhosis sets in, your liver can’t filter toxins, make proteins, or store energy properly. Some damage can heal after quitting, but advanced scarring is permanent.
Then there’s your brain. Chronic alcohol use shrinks brain tissue and messes with neurotransmitters. People often report memory lapses, trouble focusing, or mood swings. In severe cases, it leads to Wernicke-Korsakoff syndrome-a brain disorder caused by thiamine (vitamin B1) deficiency. Symptoms include confusion, loss of coordination, and even hallucinations. About 80% of people with long-term AUD are deficient in thiamine, making this a common and dangerous complication.
Your heart isn’t safe either. Heavy drinking raises blood pressure, causes irregular heartbeats (like atrial fibrillation), and increases stroke risk by 34%. It also weakens heart muscle, leading to cardiomyopathy. And your immune system? It’s compromised. Alcoholics are nearly three times more likely to get pneumonia and other serious infections because their bodies can’t fight off germs effectively.
Alcohol also increases cancer risk. Heavy drinkers face a fivefold higher chance of mouth and throat cancers, triple the risk of liver cancer, and a 12% higher risk of breast cancer for every daily drink. Even moderate drinking adds up over time.
The Hidden Costs: Mental Health and Daily Life
Alcohol doesn’t just damage your body-it rewires your life. Many people start drinking to cope with stress, anxiety, or depression. But over time, alcohol makes those problems worse. The brain’s natural production of serotonin and dopamine drops, leaving you more anxious or depressed when you’re not drinking. It becomes a cycle: drink to feel better, feel worse without it, drink again.
Relationships suffer. Jobs get lost. Finances collapse. Studies show that long-term AUD is linked to divorce, unemployment, homelessness, and legal trouble. One in three people admitted to emergency rooms for violent injuries had been drinking. And alcohol is involved in nearly 30% of all traffic deaths in the U.S.
It’s not just physical. The stigma around AUD keeps many people silent. They’re ashamed. They think they should be able to stop on their own. But AUD is not a choice. It’s a brain disease. And like any chronic illness, it needs medical care.
How Is Alcohol Use Disorder Diagnosed?
Doctors don’t diagnose AUD based on how many drinks you have per week. They use the DSM-5 criteria, which looks at 11 symptoms over a 12-month period. These include:
- Drinking more or longer than intended
- Wanting to cut down but not being able to
- Spending a lot of time drinking or recovering from its effects
- Cravings or strong urges to drink
- Drinking interferes with work, school, or family responsibilities
- Continuing to drink even when it causes relationship problems
- Giving up activities you once enjoyed because of drinking
- Drinking in dangerous situations, like driving
- Keeping drinking despite physical or mental health problems
- Developing tolerance-needing more to get the same effect
- Experiencing withdrawal symptoms when not drinking
If you have 2-3 symptoms, it’s mild AUD. 4-5 is moderate. 6 or more is severe. Most people don’t realize they’re in the moderate or severe range until they try to quit and can’t.

Treatment Isn’t One-Size-Fits-All
There’s no magic pill, but there are proven ways to recover. Treatment works best when it combines medicine, therapy, and support.
Detox is the first step-for some. If you’ve been drinking heavily for months or years, quitting cold turkey can be dangerous. Withdrawal symptoms include tremors, seizures, hallucinations, and delirium tremens (DTs), which can be fatal. Medically supervised detox in a hospital or clinic ensures safety. Doctors use benzodiazepines to calm the nervous system and prevent seizures.
Medications help you stay stopped. Three FDA-approved drugs are used to treat AUD:
- Naltrexone (ReVia, Vivitrol): Blocks the pleasurable effects of alcohol. Reduces cravings and makes drinking less rewarding.
- Acamprosate (Campral): Helps restore brain chemistry after stopping. Best for people who’ve already quit and want to avoid relapse.
- Disulfiram (Antabuse): Causes nausea, vomiting, and flushing if you drink. Works as a deterrent, not a cure.
Studies show that combining medication with therapy increases abstinence rates by 24% compared to therapy alone.
Therapy changes how you think about alcohol. Cognitive Behavioral Therapy (CBT) is one of the most effective. It helps you spot triggers-like stress, boredom, or certain people-and replace drinking with healthier responses. Motivational Enhancement Therapy (MET) helps you find your own reasons to quit, which is more powerful than someone else telling you to.
Support groups aren’t optional-they’re essential. Alcoholics Anonymous (AA) has helped millions since 1935. While its 12-step model isn’t for everyone, the peer support, structure, and accountability work. One study found 27% of members stayed abstinent after one year. Other options include SMART Recovery, which uses science-based tools, and Refuge Recovery, which blends mindfulness with addiction recovery.
New Treatments Are Changing the Game
Science is catching up. In 2022, a study in JAMA Psychiatry showed that transcranial magnetic stimulation (TMS)-a non-invasive brain stimulation technique-led to 50% abstinence rates in people with severe AUD. Another breakthrough is digital therapeutics. The FDA-approved reSET app, used with therapist support, helped 40.7% of users stay sober for 12 weeks, compared to just 17.4% in the control group.
The NIAAA’s Rethinking Drinking guide offers practical tools for cutting back or quitting, whether you’re in early recovery or just starting to think about change. It’s not about perfection-it’s about progress.

Recovery Is Possible-But It Takes Time
Some people quit cold turkey and never drink again. Others relapse multiple times before finding stability. That’s normal. Relapse doesn’t mean failure. It means the treatment needs adjusting.
Recovery isn’t just about stopping drinking. It’s about rebuilding your life. Sleep returns. Memory improves. Skin clears up. Liver enzymes start to normalize within weeks of quitting. Blood pressure drops. Depression lifts. You start remembering birthdays again. You start caring about your future.
And yes-some damage is permanent. Cirrhosis, brain shrinkage, nerve damage-these can’t always be undone. But stopping alcohol at any stage slows or halts further harm. And for many, even partial recovery means regaining control over their lives.
The biggest barrier isn’t willpower. It’s access. Only 19.2% of Americans with AUD get any kind of treatment. Insurance doesn’t cover it. Doctors don’t screen for it. Stigma keeps people silent. But change is coming. More clinics now offer medication-assisted treatment. Telehealth makes therapy accessible from home. And awareness is growing.
If you or someone you know is struggling, you’re not alone. And you don’t have to fix it alone.
Frequently Asked Questions
Can you recover from alcohol use disorder without professional help?
Some people do quit on their own, especially with mild AUD. But for moderate to severe cases, professional help greatly improves success rates. Without medical support, withdrawal can be dangerous, and relapse is common. Medications and therapy address the brain changes that make quitting so hard. Self-help works better when combined with structured support.
How long does it take for the body to heal after quitting alcohol?
Healing starts fast. Within 24 hours, your blood sugar stabilizes. After 72 hours, withdrawal symptoms peak and begin to fade. Liver enzymes drop within weeks. Sleep improves in about 2-4 weeks. After 3-6 months, many people notice better memory, clearer skin, and more energy. Liver regeneration can begin in months if cirrhosis isn’t advanced. But full brain recovery can take years, and some nerve damage may be permanent.
Is alcohol use disorder the same as alcoholism?
Yes, but the term "alcoholism" is outdated and stigmatizing. Today, doctors use Alcohol Use Disorder (AUD) to describe the full spectrum-from mild to severe. Alcoholism used to imply a moral failing. AUD is a medical diagnosis based on specific symptoms. It’s more accurate and less judgmental.
Can you drink again after recovering from AUD?
For most people with moderate to severe AUD, returning to any level of drinking leads to relapse. The brain’s reward system stays changed. Even one drink can trigger cravings and a full return to problematic use. Abstinence is the safest path. Some people with mild AUD may learn to drink moderately, but this requires careful monitoring and professional guidance. For most, lifelong abstinence is the goal.
What should I do if someone I love has AUD?
Don’t try to force them to quit. Instead, express concern without judgment. Say something like, "I’ve noticed you’ve been drinking more, and I’m worried about your health." Offer to help them find a doctor or therapist. Encourage them to use resources like the NIAAA’s Rethinking Drinking guide. Join a support group for families, like Al-Anon. Your consistent support matters more than any intervention.
Are there any natural remedies or supplements that help with AUD?
Some supplements like thiamine (B1), magnesium, and omega-3s can help repair damage caused by alcohol, especially during early recovery. But they don’t treat the addiction itself. No herb, tea, or vitamin can replace medical treatment. Relying on supplements alone is risky and can delay real recovery. Always talk to a doctor before starting any supplement, especially if you’re on medication.






Kayla Kliphardt
January 1, 2026 AT 07:12I’ve been sober 18 months now, and the thing nobody talks about is how quiet your mind gets. Not in a boring way-in a peaceful way. Like your brain finally stopped screaming for the next drink and just… breathed. I didn’t realize how much noise alcohol was making until it was gone.
Joy Nickles
January 1, 2026 AT 18:47Okay but like… why do people act like AUD is some new thing?? Like, my uncle drank himself to death in ‘98 and everyone just said ‘he had a problem’ like it was a personality flaw?? Now it’s a ‘brain disease’?? Bro, it’s always been a problem, you just wanna make it sound fancy now so you feel less guilty for not helping him…
Emma Hooper
January 2, 2026 AT 22:38Y’all need to stop romanticizing sobriety. I’ve seen too many people go from ‘I’m gonna quit and become a yoga instructor’ to ‘I drank 12 beers and passed out in a dumpster’-and then they call it ‘relapse’ like it’s a spiritual journey. It’s not. It’s addiction. It’s messy. It’s ugly. And no, you don’t get to be a ‘sober influencer’ after 6 months and sell essential oils.
Also, TMS? That’s cool, but it costs $10k. Most of us can’t afford ‘breakthroughs’-we need a clinic that takes Medicaid and doesn’t make us feel like failures for having a job.
Martin Viau
January 4, 2026 AT 21:23Canada’s got it right-universal healthcare means you don’t have to choose between rent and Vivitrol. Here in the States, you’re basically punished for being sick. My cousin had to max out three credit cards just to get detox. Meanwhile, the VA gives veterans free meds and therapy. Why? Because they’re ‘heroes.’ But the guy who drinks because his mom died? He’s just ‘weak.’
It’s not a medical issue. It’s a class issue. And we’re all just pretending otherwise.
Marilyn Ferrera
January 5, 2026 AT 06:24Thiamine deficiency is underdiagnosed. Always check B1 levels before detox. Always.
Robb Rice
January 5, 2026 AT 21:19I appreciate this post. Really well-researched. I’ve been in recovery for 7 years now. The meds helped. The therapy helped. But what kept me going? Showing up-even when I didn’t want to. Even when I felt like a fraud. Even when I didn’t believe I deserved it. That’s the real treatment. Not the pills. Not the apps. Just… showing up.
Harriet Hollingsworth
January 5, 2026 AT 21:48People who say ‘I can drink moderately now’ are lying to themselves. You can’t. You’re just lying. And you’re putting your kids at risk. You’re a danger. You need to stop. Now.
Deepika D
January 7, 2026 AT 16:40Hey, I’m from India, and here, alcohol is seen as a social evil-but no one talks about trauma. My cousin, she lost her husband in a car crash, started drinking to numb it, and no one said ‘you’re grieving,’ they said ‘she’s weak.’ But when she went to a rehab center that had counselors who spoke Hindi and understood her culture? That’s when she started healing. We need more culturally sensitive care. Not just ‘AA in English.’ We need spaces where people feel seen, not judged. And yes, I’ve seen people heal after 20 years of drinking. It’s possible. It’s not magic. It’s compassion.
Also, if you’re reading this and you’re scared to ask for help? Just text a friend. Just one word: ‘help.’ That’s enough. You don’t need to be brave. You just need to be human.
Bennett Ryynanen
January 9, 2026 AT 15:39Yo I was in the ER last month with DTs. They hooked me up to a drip and told me to ‘call a therapist.’ I didn’t have insurance. They discharged me after 48 hours. I walked out with a pamphlet and a bottle of Benadryl. That’s not treatment. That’s abandonment. If you’re gonna call it a disease, treat it like one. Not like a nuisance.