Why Documenting Generic Substitutions Matters More Than You Think
Every time a pharmacist swaps a brand-name drug for a generic version, they’re making a decision that can affect a patient’s health, safety, and trust in the system. It’s not just about saving money-though that’s a big part of it. The real risk lies in what happens when that swap isn’t properly recorded. A missing lot number, an unmarked manufacturer change, or a skipped consent signature can lead to medication errors, insurance denials, or even hospitalizations. In 2021, a patient in Ohio was admitted to the ER after a substitution of warfarin went undocumented. Their INR levels spiked because the new generic came from a different manufacturer, and no one tracked the change. That’s not a hypothetical. It happened. And it could’ve been prevented with proper documentation.
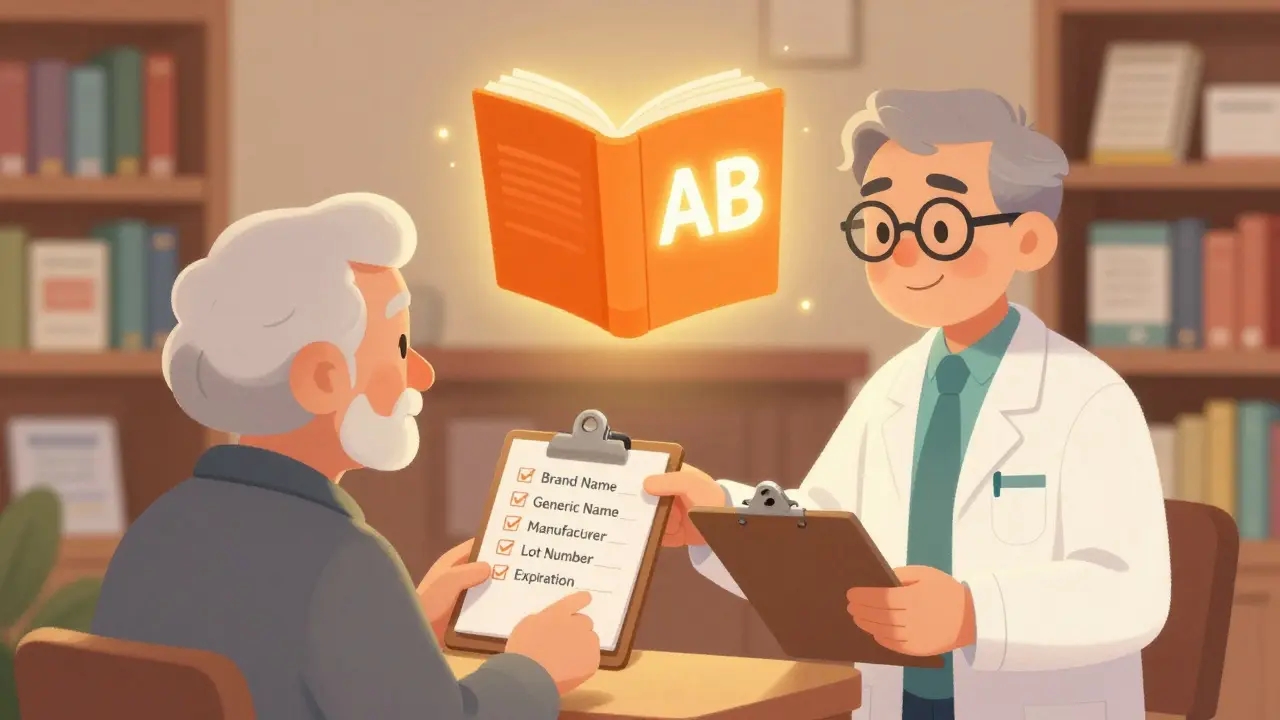
What Exactly Needs to Be Documented?
There’s no single national rule, but across 48 states, pharmacists are required to record five core details every time a generic substitution is made:
- The brand name prescribed by the doctor
- The generic name dispensed
- The manufacturer of the generic drug
- The lot number of the dispensed product
- The expiration date of the batch
That’s the baseline. Some states go further. In Oklahoma, you need written proof the patient or prescriber approved the swap. In California, as of January 2024, the substitution must be recorded in real time and made visible to the prescribing doctor through the electronic health record. If you’re working in a chain pharmacy, you might have to toggle between five different documentation templates depending on which state you’re in. That’s not inefficiency-it’s legal compliance.
When Consent Is Required (And When It’s Not)
Not every state treats patients the same way when it comes to generic substitution. Twenty-seven states let pharmacists swap generics without asking. Fourteen states require the patient to give explicit consent-usually verbal, sometimes written. Nine use a mix, like allowing substitutions for chronic meds only if the patient has been on the same generic for six months.
Here’s the kicker: states that require consent see higher prescription costs-on average $15.35 more per script in the first quarter after a brand loses exclusivity. Why? Because patients often stick with the brand they know, even if it’s more expensive. Meanwhile, states without consent rules see substitution rates jump to over 90%. But that doesn’t mean consent is bad. It means patients need to be informed. If someone’s on a narrow therapeutic index (NTI) drug like levothyroxine, phenytoin, or warfarin, even a tiny difference in absorption can be dangerous. Seventeen states have extra rules for NTI drugs: you can’t swap without telling the prescriber and getting the patient’s okay.
The Role of the Orange Book and Therapeutic Equivalence
The FDA doesn’t approve substitutions-that’s up to the states. But it does tell pharmacists what’s considered equivalent. The Orange Book (Approved Drug Products with Therapeutic Equivalence Evaluations) is the federal guide. It lists every generic drug and assigns it a code: AB means it’s therapeutically equivalent to the brand. AE means it’s not. If you’re swapping a drug coded AE, you’re breaking the law.
But here’s where things get messy. The Orange Book doesn’t officially label any drugs as NTI, even though the FDA knows they exist. That’s why state laws fill the gap. Pharmacists have to know the difference between a drug that’s just bioequivalent and one that’s clinically sensitive. A 2011 study in PubMed Central warned that bioequivalence doesn’t always mean therapeutic equivalence-especially for drugs with a narrow window between effective and toxic doses. Documentation isn’t just paperwork. It’s your safety net.
Electronic Systems and the Burden of Compliance
Most pharmacies use electronic systems to track substitutions. But not all systems are built the same. Epic Systems reported in 2023 that 32% of pharmacies using their platform had to build custom fields just to meet state requirements. That’s not a flaw in the software-it’s a flaw in the patchwork of state laws. One pharmacy in Texas might need to log a prescriber’s approval code. Another in New York might need to attach a scanned consent form. A new pharmacist can take 4 to 6 weeks just to learn the rules for their state.
And timing matters. Forty-one states require documentation to be completed within 24 hours of dispensing. Miss that window, and you risk audit penalties, insurance rejections, or even license issues. The American Pharmacists Association found that 68% of pharmacists find documentation “moderately burdensome,” but 92% agree it’s necessary. Why? Because 23% say they’ve prevented an adverse event just by catching a mismatch in lot numbers or manufacturers during a routine record check.
What Happens When Documentation Fails
Bad documentation doesn’t just mean a denied insurance claim. It can cost lives. The Journal of the American Pharmacists Association documented a case where a patient on warfarin was switched to a different generic without documentation. Their INR went from 2.5 to 5.8 in two weeks. They had a brain bleed. The pharmacy had no record of the substitution. No one knew what had changed. The patient survived, but only after a $120,000 hospital stay.
On the flip side, a 2022 study across 150 community pharmacies showed that when substitution decisions were fully documented, medication errors dropped by 17.3% in six months. That’s not a small number. That’s hundreds of potential hospitalizations avoided. The same study found that when pharmacists documented the reason for a substitution-like “brand unavailable” or “patient requested generic”-it improved communication with prescribers and reduced follow-up calls by 40%.
What’s Changing in 2024 and Beyond
The landscape is shifting. California’s SB 564, effective January 1, 2024, requires real-time electronic documentation accessible to prescribers. That’s a big step toward transparency. The FDA’s GDUFA III rules, rolled out in late 2022, now require manufacturers to submit more detailed bioequivalence data for complex generics-like extended-release pills or inhalers. That means pharmacists will soon have more data to work with, but also more to document.
Blockchain is being tested. A pilot by the National Pharmaceutical Council showed a 22% drop in documentation errors when substitution records were stored on a blockchain ledger. It’s not mainstream yet, but it’s coming. The ASPE is drafting national guidelines for substitution documentation, expected in mid-2024. If adopted, it could cut the current 50-state patchwork down to a single standard. That would save the healthcare system an estimated $4.2 billion a year by reducing errors and hospitalizations.

How to Get It Right Every Time
If you’re a pharmacist, here’s your checklist:
- Check the Orange Book before you swap-confirm the AB rating.
- Know your state’s consent rules-ask if required, don’t assume.
- Record all five core details: brand, generic, manufacturer, lot, expiration.
- For NTI drugs, always notify the prescriber and get patient consent.
- Document within 24 hours-don’t wait until the end of the shift.
- Use your pharmacy system’s substitution field-don’t type notes in free text.
- If something feels off-like a new generic causing unexpected side effects-document it and report it.
Documentation isn’t busywork. It’s your professional responsibility. It’s how you protect your license, your patients, and your pharmacy from liability. In a system where 90% of prescriptions are filled with generics, the paper trail is the only thing standing between a safe outcome and a preventable tragedy.
Frequently Asked Questions
Do I need patient consent for every generic substitution?
No-not in every state. Twenty-seven states allow pharmacists to substitute without consent, while 14 require explicit patient agreement. Nine states use a hybrid model, often requiring consent for chronic medications or NTI drugs. Always check your state’s pharmacy board rules before making a substitution.
What if the generic drug comes from a different manufacturer than the last fill?
You must document the new manufacturer and lot number. Even if the generic is therapeutically equivalent (AB-rated), switching manufacturers can affect absorption-especially for NTI drugs like levothyroxine or warfarin. Some patients report changes in how they feel after a manufacturer switch. Documenting this helps track patterns and alerts prescribers if issues arise.
Can I substitute a brand-name drug if the prescriber wrote “Do Not Substitute”?
No. If the prescriber writes “Do Not Substitute” or “Dispense as Written” on the prescription, you are legally required to fill it exactly as written. This is true in all 50 states. Overriding this instruction can result in disciplinary action, civil liability, or even loss of your license.
Are generic drugs really as safe as brand-name drugs?
For most drugs, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also meet strict bioequivalence standards. However, for narrow therapeutic index (NTI) drugs, small differences in absorption can matter. That’s why documentation is critical-it lets you and the prescriber monitor for any unexpected changes in patient response.
What should I do if a patient reports a problem after a generic substitution?
First, review your documentation: did you record the manufacturer and lot number? Did you check the Orange Book? Then, contact the prescriber immediately and document the patient’s symptoms. Report the issue to the FDA’s MedWatch program. The World Medical Association recommends that physicians report any adverse reactions linked to substitution to national regulatory authorities. Your documentation is your evidence-and it could prevent harm to others.
Is there a national standard for documenting substitutions?
Not yet. Each state has its own rules, which is why national pharmacy chains struggle with consistency. But the Model State Pharmacy Act (2022) recommends uniform standards, and 12 states have already adopted them. The ASPE is drafting national guidelines expected in mid-2024. If passed, this could reduce the current patchwork of 50 different systems.
Next Steps for Pharmacists
If you’re new to the job, spend your first month mapping out your state’s substitution laws. Use the National Community Pharmacists Association’s online tool-it’s updated quarterly and shows exactly what you need to document. If you’re managing a pharmacy, audit your EHR system. Make sure substitution fields are mandatory and that lot numbers and manufacturers are captured automatically. Train your technicians: they’re the ones entering most of this data. And if you’re ever unsure, don’t guess. Call your state board of pharmacy. Better to ask once than to risk a patient’s life.






Diksha Srivastava
February 1, 2026 AT 10:32Bobbi Van Riet
February 2, 2026 AT 02:32Rob Webber
February 3, 2026 AT 19:08Amy Insalaco
February 4, 2026 AT 14:58Lily Steele
February 5, 2026 AT 03:31Rohit Kumar
February 5, 2026 AT 04:51Marc Bains
February 6, 2026 AT 18:51calanha nevin
February 8, 2026 AT 05:33Sidhanth SY
February 9, 2026 AT 01:28Melissa Cogswell
February 9, 2026 AT 07:16Natasha Plebani
February 10, 2026 AT 17:16Blair Kelly
February 11, 2026 AT 01:29Kelly Weinhold
February 11, 2026 AT 17:39Katie and Nathan Milburn
February 12, 2026 AT 10:05