Autoimmune hepatitis is a serious but treatable condition where the body’s own immune system attacks the liver. Unlike viral hepatitis, it’s not caused by an infection-it’s a misfire. The immune system sees liver cells as foreign invaders and starts destroying them. Left untreated, this inflammation can lead to scarring, cirrhosis, and even liver failure. The good news? With the right diagnosis and treatment, most people can stop the damage and live normal, healthy lives.
How Is Autoimmune Hepatitis Diagnosed?
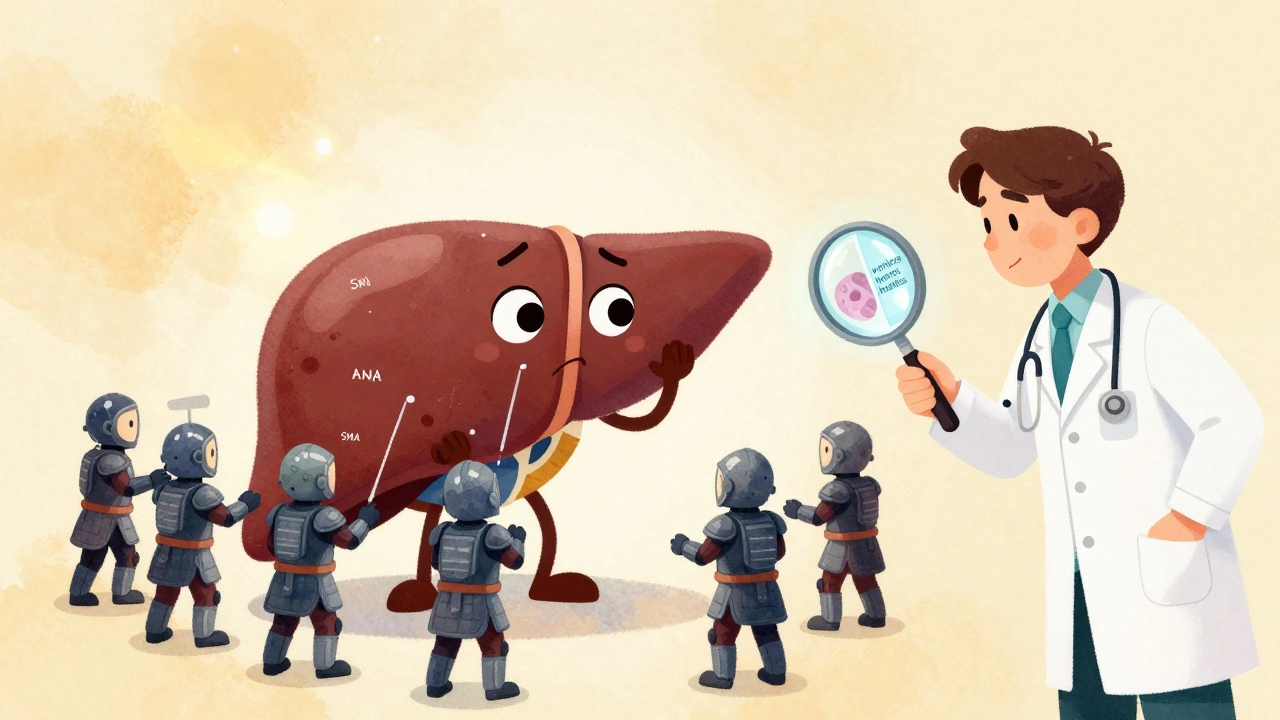
There’s no single test that confirms autoimmune hepatitis. Doctors have to piece together clues from blood work, imaging, and a liver biopsy. That’s because symptoms are often vague-fatigue, joint pain, dark urine, or jaundice-and can look like other liver diseases. Blood tests are the first step. Elevated liver enzymes-ALT and AST-are common, often 5 to 10 times higher than normal. Another key marker is immunoglobulin G (IgG), which is usually more than 1.5 times the upper limit of normal. Autoantibodies like antinuclear antibodies (ANA) or smooth muscle antibodies (SMA) are also found in about 80% of cases. These aren’t diagnostic on their own, but when combined with other signs, they point strongly to autoimmune hepatitis. The gold standard for diagnosis is a liver biopsy. A small sample of liver tissue is taken using a thin needle, usually guided by ultrasound. Under the microscope, pathologists look for a specific pattern called interface hepatitis-where immune cells invade the border between liver tissue and blood vessels. This pattern is almost unique to autoimmune hepatitis. The biopsy also shows how much scarring (fibrosis) is already present, which helps predict how urgent treatment needs to be. To make things even clearer, doctors use the Revised International Autoimmune Hepatitis Group (IAIHG) scoring system. It gives points for blood test results, antibody levels, biopsy findings, and rules out other causes like hepatitis B or C. A score over 15 means probable autoimmune hepatitis; over 20 confirms it. This system reduces guesswork and ensures patients aren’t misdiagnosed.Why Steroids Are the First-Line Treatment
Since the 1970s, corticosteroids have been the backbone of autoimmune hepatitis treatment. Prednisone (or its active form, prednisolone) works fast-often within two weeks. It shuts down the overactive immune response that’s damaging the liver. In fact, 80 to 90% of patients show clear improvement in liver enzyme levels within that short window. That rapid response is so consistent that doctors often use it as a diagnostic clue: if steroids improve the liver tests, it’s likely autoimmune hepatitis. But steroids come with serious side effects. Weight gain, mood swings, high blood sugar, bone thinning, and cataracts are common. About 70% of people on steroid-only treatment develop at least one major side effect within five years. That’s why doctors don’t keep patients on high doses for long. The standard starting dose is 0.5 to 1 mg per kilogram of body weight per day-up to 60 mg daily. After about six to eight weeks, the dose is slowly reduced. The goal is to get down to 10 to 15 mg per day within two months. This tapering is critical. Too fast, and the disease can flare. Too slow, and side effects pile up.The Role of Azathioprine: Steroid-Sparing and Long-Term Control
Azathioprine (sold as Imuran or generic versions) is almost always added to steroid therapy. It doesn’t work as fast as steroids, but it’s a game-changer for long-term management. Azathioprine suppresses the immune system more gently and allows doctors to cut steroid doses by 70 to 80% within six months. That dramatically reduces side effects. The usual starting dose is 50 mg per day, increased gradually to 1 to 2 mg per kilogram per day (up to 150 mg). It’s taken daily, often for years. The key advantage? It helps maintain remission. Studies show that patients on combination therapy (steroids + azathioprine) are far less likely to relapse than those on steroids alone. But azathioprine isn’t risk-free. It can lower white blood cell counts, cause nausea, or rarely, trigger pancreatitis. About 12% of patients experience bone marrow suppression. That’s why testing for TPMT enzyme levels is now standard before starting the drug. TPMT is a liver enzyme that breaks down azathioprine. People with low or absent TPMT activity can’t process the drug safely and risk life-threatening toxicity. Testing for this takes just a few days and costs $250-$400 in the U.S.-a small price to avoid hospitalization.
What Does Successful Treatment Look Like?
Success isn’t just about feeling better. It’s measured by lab results and liver tissue changes. Complete biochemical response means ALT and AST levels return to normal, and IgG drops back to baseline. That happens in 60 to 80% of patients within 18 to 24 months. Even better-histological remission. That means a repeat liver biopsy shows no more interface hepatitis. About half to two-thirds of patients reach this stage after two to three years of treatment. In some cases, fibrosis actually reverses. One patient reported going from F3 (advanced scarring) to F0 (no scarring) on biopsy after two years on low-dose steroids and azathioprine. But remission doesn’t mean cure. Most patients-60 to 80%-need to stay on some form of treatment indefinitely. Stopping therapy too soon leads to relapse in 50 to 90% of cases. Even if blood tests look perfect, the immune system can wake up again.What If Treatment Doesn’t Work?
About 10 to 15% of patients don’t respond well to steroids and azathioprine. These are called treatment failures. Signs include persistent high liver enzymes after 12 to 18 months, or worsening symptoms despite treatment. The next step is usually switching to mycophenolate mofetil (CellCept). It’s taken twice daily and has fewer side effects than azathioprine for some people. It’s especially useful if azathioprine caused pancreatitis or low blood counts. Another option is calcineurin inhibitors like tacrolimus or cyclosporine, which are stronger immunosuppressants. Newer drugs are on the horizon. Obeticholic acid (Ocaliva), originally for primary biliary cholangitis, showed promise in phase 3 trials for AIH, with a 42% complete response rate compared to 28% with standard therapy. JAK inhibitors like tofacitinib and monoclonal antibodies targeting interleukin-6 are also being tested in early trials. These could change the game for patients who don’t respond to current treatments.Monitoring and Prevention: What You Need to Do
Regular check-ins are non-negotiable. Blood tests for liver enzymes and IgG should be done every 2 to 4 weeks during the first few months, then every 3 months once stable. A repeat liver biopsy is recommended after 18 to 24 months to check for histological improvement. Before starting immunosuppressants, testing for hepatitis B is mandatory. About 15 to 20% of people carry hidden hepatitis B virus. If they start steroids or azathioprine, the virus can reactivate and cause sudden, life-threatening liver failure. If HBsAg or anti-HBc is positive, antiviral drugs like tenofovir are started first. Vaccinations matter too. Hepatitis A and B vaccines should be given before treatment begins. Once you’re on immunosuppressants, vaccines don’t work as well-efficacy drops from 90% to 40-60%. Don’t wait until you’re already on medication to get them.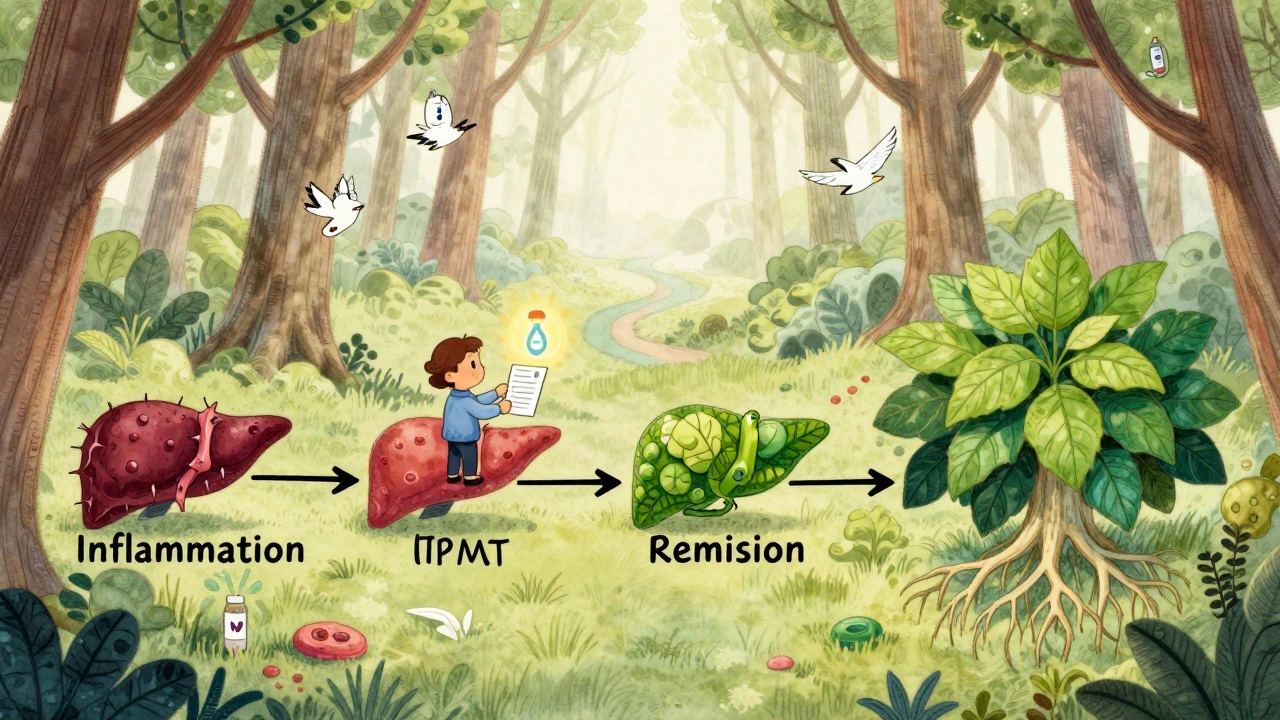
Real Patient Experiences and Challenges
Patients don’t just deal with medical facts-they live with side effects. One person described steroid use as making them look unrecognizable: "moon face," 30 pounds of fluid weight in weeks, and sleepless nights. Another had pancreatitis from azathioprine and had to switch to mycophenolate after 18 months of trial and error. But there are wins too. Many report feeling like themselves again after a year. One patient said, "My biopsy showed complete fibrosis reversal." That’s not just hope-it’s science. The biggest hurdle? Adherence. Only 55% of patients stick with steroid-only treatment. But with combination therapy, adherence jumps to 75%. Why? Because side effects are manageable when steroid doses are low.What’s New in 2025?
The 2025 European Association for the Study of the Liver (EASL) guidelines made big changes. First, they stopped recommending autoantibody subclassification. Whether you have ANA or LKM1 doesn’t change your treatment plan anymore. Second, they extended the window for assessing treatment response from 6 to 6-12 months. That’s more realistic-some people just take longer to respond. Also, TPMT testing is now considered essential. In Europe, 78% of centers do it. In the U.S., it’s only 45%. That gap needs closing. Preventing toxicity is easier than treating it. Research is moving fast. Trials are testing whether patients with sustained remission can safely stop treatment. Early data suggests up to 65% stay in remission after stopping-much better than the old 35%. If confirmed, this could mean some people eventually get off drugs entirely.Final Thoughts: Hope Is Real
Autoimmune hepatitis is not a death sentence. It’s a chronic condition, yes-but one that responds well to treatment. The combination of steroids and azathioprine has saved thousands of lives since the 1970s. Newer drugs are coming, and monitoring is smarter than ever. The key is early diagnosis and sticking with treatment. Side effects are tough, but they’re often worse than the disease. With the right team and the right plan, most people with autoimmune hepatitis go on to live full, active lives. The liver can heal. The immune system can be reined in. And with ongoing research, the future looks even brighter.Can autoimmune hepatitis be cured?
Autoimmune hepatitis cannot be cured in the traditional sense, but it can be effectively controlled. With long-term treatment, most patients achieve remission-meaning liver inflammation stops, liver enzymes return to normal, and scarring may even reverse. However, stopping treatment often leads to relapse in 50-90% of cases. For this reason, many patients need to stay on low-dose medication for life.
How long does it take for azathioprine to work?
Azathioprine doesn’t work quickly. It usually takes 2 to 6 months to show full effect. That’s why it’s always started alongside steroids, which work within weeks. Azathioprine’s job is to maintain remission and let doctors reduce steroid doses safely. Patience is key-rushing to stop steroids too soon can trigger a flare.
Is a liver biopsy always necessary?
Yes, a liver biopsy is still required for a definitive diagnosis. Blood tests and autoantibodies can suggest autoimmune hepatitis, but only a biopsy can confirm the classic pattern of interface hepatitis. This is critical to rule out other liver diseases like fatty liver, alcohol-related damage, or drug-induced injury. Even if the blood work looks clear, skipping the biopsy risks misdiagnosis.
Can I drink alcohol with autoimmune hepatitis?
No. Alcohol adds extra stress to an already inflamed liver and speeds up scarring. Even small amounts can worsen disease progression. Abstinence is strongly recommended for all patients with autoimmune hepatitis, regardless of how well their condition is controlled. The liver needs every advantage to heal.
What are the signs that treatment isn’t working?
If your ALT and AST levels remain elevated after 6-12 months of treatment, or if symptoms like fatigue and jaundice return, your treatment may not be working. A repeat biopsy showing persistent interface hepatitis is the clearest sign. Your doctor may then switch you to a second-line drug like mycophenolate or a calcineurin inhibitor. Don’t wait-early intervention prevents permanent damage.
Can I get pregnant while on azathioprine or steroids?
Yes, many women with autoimmune hepatitis have healthy pregnancies while on low-dose steroids and azathioprine. In fact, staying on treatment during pregnancy reduces the risk of disease flare, which is more dangerous to mother and baby than the medications. Azathioprine is considered relatively safe in pregnancy, and prednisone crosses the placenta minimally. Always consult your hepatologist and obstetrician before planning pregnancy.







Jimmy Jude
December 4, 2025 AT 06:14So let me get this straight - we’re poisoning people with steroids just to keep their immune system from killing their own liver? And we call this medicine? I mean, if your body’s fighting a war, why are we arming the enemy and then blaming them for the collateral damage? This isn’t treatment, it’s a hostage negotiation with your own cells.
Mark Ziegenbein
December 4, 2025 AT 22:30The entire paradigm of autoimmune hepatitis management is built on a 1970s pharmacological compromise - prednisone as a blunt instrument to suppress inflammation and azathioprine as a slow-burning fuse to prevent relapse - yet we still lack a single biomarker that predicts who will achieve true histological remission versus who will spiral into steroid dependence or drug-induced cytopenia. The IAIHG scoring system is elegant in theory but fails to account for epigenetic variability, metabolic polymorphisms, or the gut-liver axis modulation that may underlie treatment resistance. We are treating a symptom cluster with a sledgehammer while ignoring the architecture of autoimmunity itself.
Juliet Morgan
December 6, 2025 AT 09:53I was diagnosed 3 years ago and honestly? This post saved my life. I thought I was just tired but turns out my liver was screaming. The biopsy scared me but knowing what they were looking for made it less terrifying. Azathioprine made me nauseous at first but after 2 months I felt like me again. You’re not alone.
Harry Nguyen
December 7, 2025 AT 04:39Of course the medical establishment wants you to stay on drugs forever - they make billions off it. Why would they want a cure when they’ve got a cash cow? You think they’d test real alternatives if it didn’t mean losing their gravy train? The FDA’s just a pharmaceutical puppet. Get off the pills. Try turmeric. Or better yet - move to a country where they don’t poison you with steroids.
Stephanie Fiero
December 7, 2025 AT 22:18Guys I just wanna say - if you're on azathioprine and your WBC drops, DON'T IGNORE IT. I did. Ended up in the ER with sepsis. TPMT test is NOT optional. It's literally life or death. My doctor didn't even mention it until I asked. Advocate for yourself. You got this.
Laura Saye
December 9, 2025 AT 10:40The concept of remission in autoimmune disease is paradoxical - it implies cessation of pathology without resolution of etiology. We are not curing the immune system’s misrecognition; we are merely dampening its expression. The fibrosis reversal observed in some patients suggests remarkable hepatic plasticity - a testament to the liver’s intrinsic regenerative capacity when inflammation is quelled. Perhaps true healing lies not in suppression, but in restoration of immune tolerance - a frontier still largely unexplored.
Stephanie Bodde
December 9, 2025 AT 18:39Thank you for writing this. I cried reading the part about fibrosis reversal. My biopsy last month showed F1 now - from F3. I’m on low-dose steroids + azathioprine and it’s been 2 years. I still have side effects, but I can play with my kids again. 🙏❤️
Mellissa Landrum
December 10, 2025 AT 09:45Did you know the WHO is hiding the truth? Steroids cause more liver damage than the disease itself. The real cause? Glyphosate in your food. The FDA knows. Big Pharma knows. They don’t want you to know. Get organic. Stop eating processed crap. Your liver will thank you. And no - I don’t work for the government.
luke newton
December 11, 2025 AT 04:22My uncle died of liver failure at 48. They told him it was autoimmune. He was on prednisone for 7 years. He looked like a balloon. He couldn’t walk. He couldn’t sleep. He died anyway. This whole system is a scam. You’re being sold a slow death with a side of moon face. Wake up.
James Moore
December 12, 2025 AT 10:41It is, in fact, a remarkable demonstration of medical science’s capacity for incremental progress - the transition from monotherapy with corticosteroids to combination immunosuppression with azathioprine represents not merely a therapeutic optimization, but a paradigmatic shift in the conceptualization of chronic autoimmune disease - from acute suppression to sustained modulation - yet the persistent reliance on invasive biopsy as the gold standard reveals an institutional inertia that resists the advent of non-invasive biomarkers, such as serum microRNA profiles or elastography-based fibrosis quantification, which, though promising, remain underutilized in clinical practice due to reimbursement barriers and entrenched diagnostic dogma.
Carole Nkosi
December 13, 2025 AT 01:04Why do we still use steroids? They’re outdated. We have biologics now. Why are we torturing patients with weight gain and diabetes when we could use targeted therapy? This is 2025. We’re still using 1970s tools because the system is broken. I’m from South Africa - we don’t have access to TPMT testing. People die here because of bureaucracy. This isn’t medicine. It’s a privilege.
Philip Kristy Wijaya
December 13, 2025 AT 09:24Let me be perfectly clear - the notion that autoimmune hepatitis can be managed with pharmacological suppression is a profound ethical failure of modern hepatology. The liver is not a broken machine to be patched with immunosuppressants; it is a sentient organ embedded within a systemic ecosystem of microbiota, neuroendocrine signaling, and metabolic homeostasis. To treat it as a discrete target is to commit epistemological violence upon the patient. The true solution lies not in drug cocktails, but in dietary rewilding, circadian entrainment, and vagal nerve stimulation - modalities dismissed as quackery by the medical industrial complex because they cannot be patented.
Mark Curry
December 15, 2025 AT 02:22I’ve been on azathioprine for 4 years. I still take my pills every morning. I don’t feel perfect, but I don’t feel sick either. I walk my dog, I cook, I laugh. That’s enough. Thanks for the info - it helped me feel less alone.