
Every year, medication adherence fails for millions of people-not because they don’t care, but because they can’t afford it. You take your pills every day. You know they’re important. But when the pharmacy bill hits $150 for a 30-day supply, and your paycheck barely covers rent and groceries, something has to give. That’s not laziness. That’s survival. And it’s happening more than you think.
Why Cost Stops People from Taking Their Medication
It’s not just about being broke. It’s about how the system is built. High deductibles, surprise copays, and tiered formularies mean two people with the same insurance can pay wildly different amounts for the same drug. A 2022 analysis of 71 studies found that 84% showed a direct link between higher out-of-pocket costs and worse adherence. The more you pay, the less likely you are to take your medicine.
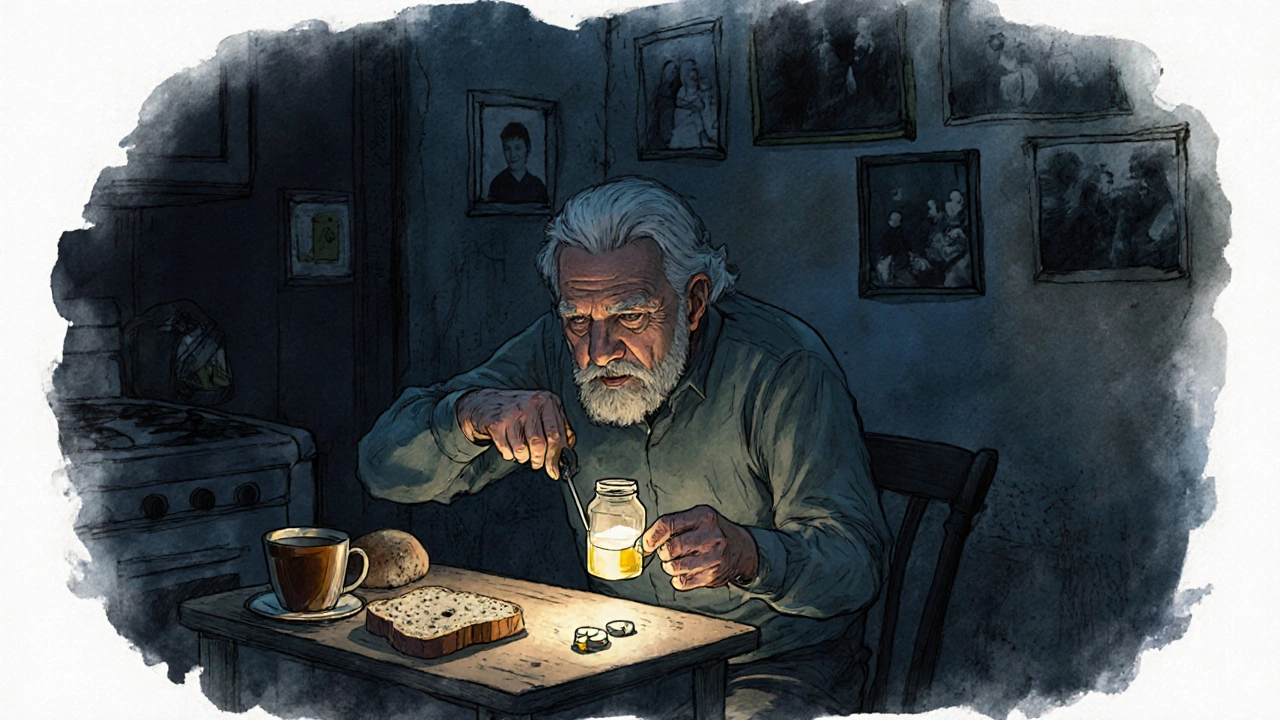
For many, the choice isn’t between health and money-it’s between health and food, heat, or rent. One 62-year-old Medicare beneficiary told Kaiser Health News she pays $350 a month for her meds after insurance. That’s more than her electric bill. She skips doses. She cuts pills in half. She chooses which pill to skip based on which condition feels worse that week.
Cost-related nonadherence isn’t rare. The CDC found that 8.2% of working-age adults in the U.S. didn’t take their meds as prescribed because of cost. That’s over 1 in 12 people. And it’s worse for low-income groups. People earning under $25,000 a year are more than three times as likely to skip doses than those making over $75,000.
Cardiovascular drugs are especially sensitive to price. Patients with high blood pressure or cholesterol often cut back because they don’t feel sick-until they do. One study showed that when copays jumped from $10 to over $50, adherence dropped by 15-20%. That’s not a small dip. That’s a cliff.
What People Do When They Can’t Afford Their Meds
People don’t just stop taking pills. They get creative. And desperate.
- They split pills-even when the drug isn’t scored.
- They delay refills, hoping symptoms get better.
- They call their doctor asking for samples, hoping to stretch the supply.
- They switch to cheaper generics-even if their doctor didn’t recommend it.
- They use GoodRx or SingleCare to compare prices across pharmacies.
One Reddit user shared that even with insurance, their insulin cost $800 a month. Another said they took half their daily dose to make it last two weeks. These aren’t outliers. They’re common stories.
And then there’s the sticker shock. Forty-one percent of patients say the price at the pharmacy was way higher than what their doctor told them. That’s because doctors often don’t know the real cost. Insurance networks change. Pharmacy deals shift. And unless a prescriber checks the formulary in real time, they’re guessing.
How to Get Help: Real Solutions That Work
There are ways out. You don’t have to choose between your health and your bills. Here’s what actually works.
1. Talk to Your Doctor
Don’t wait until you’re skipping doses. Say it out loud: “I can’t afford this.” Doctors aren’t shocked by this. In fact, 65% now ask about cost during visits-up from 42% just five years ago. Ask for:
- A generic version
- A drug on your insurer’s discount list
- A 90-day supply (often cheaper per pill)
- A sample pack to bridge the gap
Some doctors have access to real-time benefit tools that show you the exact price before they write the script. Ask if your clinic uses one.
2. Use Patient Assistance Programs
Pharmaceutical companies run these programs to help low-income patients. In 2022, they helped 1.8 million Americans. Eligibility? Usually income under 400% of the federal poverty level-that’s $55,520 for one person in 2023.
For example, a type 2 diabetes patient was paying $500 a month for insulin. After enrolling in the manufacturer’s program, her cost dropped to $25. Her adherence jumped from 60% to 95%.
Start with Partnership for Prescription Assistance or RxAssist. They’ll match you to programs you qualify for.
3. Try GoodRx or SingleCare
These free apps compare prices across pharmacies. Sometimes the cash price is lower than your insurance copay. One user saved 78% on metformin by paying $12 instead of using insurance. Thirty-five million Americans use these tools every month.
Pro tip: Bring the coupon to the pharmacy. Don’t assume the pharmacist will know. Sometimes they need to manually enter the code.
4. Medicare? Use Extra Help
If you’re on Medicare Part D and your income is low, you may qualify for Extra Help. In 2023, it covers up to $5,000 in annual drug costs. That means you pay $0-$10 for most prescriptions. Apply at ssa.gov or call 1-800-772-1213.
5. Ask About Mail-Order Pharmacies
Many insurers offer 90-day mail-order options. These often cut per-pill costs by 20-30%. You get your meds delivered. No trips to the pharmacy. No surprise bills.
What’s Changing in 2025 and Beyond
The system is starting to bend under pressure. The Inflation Reduction Act is changing Medicare Part D. Starting in 2025, out-of-pocket drug costs for seniors will be capped at $2,000 a year. The infamous “donut hole” is gone. And for high-cost drugs, you’ll be able to pay in monthly installments instead of one big bill.
More generics are hitting the market too. In 2022, the FDA approved 1,123 new generic drugs. That’s more competition. That’s lower prices.
But experts warn: without real drug pricing reform, these fixes won’t be enough. The Congressional Budget Office predicts U.S. drug spending will hit $1.1 trillion by 2031. That’s more than double what it was in 2022. And if prices keep rising, even more people will be forced to choose.

What You Can Do Right Now
You don’t need to wait for policy changes. Start today.
- Look at your last prescription receipt. Is the price higher than you expected?
- Search your drug name on GoodRx or SingleCare. Compare prices at three nearby pharmacies.
- Call your doctor’s office. Say: “I’m struggling to afford my meds. Can we talk about cheaper options?”
- Visit RxAssist.org. Fill out the form. It takes 5 minutes.
- If you’re on Medicare, check if you qualify for Extra Help. You might be eligible even if you didn’t think you were.
Medication adherence isn’t about willpower. It’s about access. And if you’re skipping doses because of cost, you’re not alone. You’re not failing. You’re stuck in a system that wasn’t built for people like you. But there are tools. There are programs. There’s help. You just have to ask.
Why do some people skip doses even when they know it’s dangerous?
People don’t skip doses because they’re careless-they do it because they have to. When a medication costs more than a week’s groceries, choosing between health and food isn’t a choice-it’s a survival tactic. Studies show that cost is the top reason for nonadherence, even more than forgetting or not understanding the treatment. It’s not about discipline. It’s about dollars.
Can I use GoodRx even if I have insurance?
Yes, and you should always check. Sometimes the cash price with a GoodRx coupon is lower than your insurance copay, especially for generic drugs. Pharmacies can’t always combine insurance with coupons, but you can choose which payment method to use. Always ask the pharmacist: “Can I pay cash with this coupon instead of using insurance?”
Do all drug companies offer patient assistance programs?
Most major manufacturers do-especially for chronic condition drugs like insulin, blood pressure meds, and antidepressants. Smaller or newer companies may not. But if you’re on a brand-name drug, it’s worth checking. The Partnership for Prescription Assistance has a database of over 475 programs. You don’t need to know which one to ask for-they’ll match you.
What if my doctor won’t switch my prescription to a cheaper one?
You have the right to ask. If your doctor says no, ask why. Is it because the alternative isn’t as effective? Or because they’re not familiar with cheaper options? You can also ask for a referral to a pharmacist who specializes in medication cost management. Many hospitals have clinical pharmacists who help patients find affordable alternatives.
Is it safe to split pills to save money?
It depends. Some pills are designed to be split-like those with a score line. Others, like extended-release capsules or coated tablets, can be dangerous if split. Splitting them can change how the drug is absorbed, leading to under- or overdosing. Never split a pill without checking with your pharmacist first. Better yet, ask for a lower-dose pill instead.
How do I know if I qualify for Medicare’s Extra Help program?
For 2023, you qualify if your income is below $21,870 for an individual or $29,580 for a couple, and your resources (savings, investments, property) are under $16,620 (or $33,240 for couples). Even if you think you make too much, apply anyway-some states have expanded eligibility. You can apply online at SSA.gov or call 1-800-772-1213. It takes about 10 minutes.
Why are some medications so expensive even when they’ve been around for decades?
Many older drugs, like insulin or metformin, were developed decades ago but are now sold under brand names with little competition. Manufacturers raise prices because they can-there’s no law forcing them to lower them. Between 2007 and 2017, insulin list prices tripled, even though the cost to produce it barely changed. Generic versions exist, but sometimes they’re still priced high because of how the supply chain works. That’s why using GoodRx or patient programs is critical.
Final Thought: You’re Not Alone
Medication adherence isn’t just a medical issue. It’s a human one. You’re not failing. You’re navigating a system that wasn’t designed for people with limited income. But you don’t have to do it alone. Thousands of people are in the same boat. And there are real, proven ways to cut costs-right now. Start with one step: check your next prescription on GoodRx. Call your doctor. Apply for one program. It might not fix everything. But it might just keep you alive.



Nicole Ziegler
November 20, 2025 AT 04:20This hit me right in the feels. My mom skips her blood pressure pills every other month to afford her insulin. She says she’s ‘just being smart’ but I know she’s scared. 🥺
Bharat Alasandi
November 21, 2025 AT 06:45Bro in India we got the same problem but worse. My uncle takes half a 50mg metformin tablet because the full dose costs 300 rupees. He says ‘if I feel fine, I don’t need the full dose.’ No doctor ever asked him if he could afford it. 😔
Ravi boy
November 21, 2025 AT 13:08goodrx saved my life last year on my antidepressants. paid 12 bucks cash instead of 80 with insurance. pharmacy guy was like ‘wait u can do that?’ yeah bro its 2024 not 2004
Liam Strachan
November 22, 2025 AT 03:47It’s wild how we treat medication like a luxury item. In the UK, we’ve got free prescriptions for chronic conditions - and yes, people still forget to take them. But at least they don’t have to choose between meds and heating the house. This isn’t just a US problem - it’s a capitalism problem.
Aruna Urban Planner
November 23, 2025 AT 01:34There’s a systemic failure here that’s being framed as individual responsibility. People aren’t ‘noncompliant’ - they’re rationing survival. The medical-industrial complex profits from chronic illness, and the pricing structure is designed to exclude. We talk about adherence like it’s a behavioral issue, when it’s a structural one. Until we decouple healthcare from profit motives, no amount of GoodRx coupons will fix the root.
Pharmaceutical patents exist to delay generics, not to incentivize innovation. The $500 insulin that costs $5 to produce? That’s not market failure - that’s market design. And the fact that doctors are only now being trained to ask about cost? That’s 20 years too late.
There’s a reason why countries with universal healthcare have higher adherence rates. It’s not because their citizens are more disciplined. It’s because they’re not forced to gamble with their lives every time they walk into a pharmacy.
When a 62-year-old woman chooses which chronic condition to let worsen this week based on which pill she can afford - that’s not a personal failure. That’s a moral failure of the entire system.
And yes, patient assistance programs help - but they’re band-aids on a hemorrhage. They require paperwork, eligibility checks, and time people don’t have. Meanwhile, the same companies that offer these programs spend billions on shareholder dividends and executive bonuses.
We need price caps. We need mandatory transparency. We need public manufacturing of essential drugs. We need to treat medicine like a human right, not a commodity.
Until then, I’ll keep sharing GoodRx links and calling doctors on their silence. But let’s be clear: this isn’t about individual solutions. It’s about collective action.
Shiv Karan Singh
November 24, 2025 AT 11:06lol u think this is bad? wait till u see how people in india buy fake meds off the street because real ones r too expensive. at least u got goodrx. we got whatsapp pharmacies. 💀
Matthew Karrs
November 26, 2025 AT 00:08Let’s be real - the whole ‘patient assistance program’ thing is a PR stunt. Big Pharma knows people will beg for scraps so they can keep the prices sky-high. They’re not helping you - they’re protecting their stock price. And don’t get me started on how they lobby to block generic competition. This isn’t charity. It’s calculated cruelty.
Matthew Peters
November 27, 2025 AT 10:55I just called my doctor and asked if she could switch me to a cheaper med. She looked at me like I’d asked her to perform surgery with a butter knife. Then she said ‘I’ll check the formulary’ - and 10 minutes later, I had a $12 generic. I cried in the parking lot. Nobody talks about how terrifying it is to ask for help. But you have to. It’s worth it.
Gerald Cheruiyot
November 27, 2025 AT 22:50When I was in grad school in 2018 I had to choose between my asthma inhaler and my rent. I chose rent. I ended up in the ER. The bill was $4000. Insurance covered $3900. I paid $100. That’s the same price as my inhaler. I’ve never forgotten that. If you’re reading this and you’re struggling - you’re not weak. You’re surviving. And you deserve better than this broken system.
Kristi Bennardo
November 29, 2025 AT 00:34This entire article reads like a corporate-sponsored PR campaign disguised as advocacy. Patient assistance programs? GoodRx? These are not solutions - they are distractions. They keep people docile while the real issue - the criminal monopolization of life-saving drugs - goes unchallenged. The Inflation Reduction Act’s $2,000 cap? That’s still 20 times what it should be. The FDA approves generics, but the supply chain is rigged. This isn’t about access - it’s about control. And those who profit from this system are not just guilty - they are morally bankrupt.