Most people never hear about subclinical hyperthyroidism until it shows up on a routine blood test. Your TSH is low, but your T3 and T4? Perfectly normal. No weight loss. No shaky hands. No racing heart. So why should you care? Because even when you feel fine, your heart might be paying a price.
What Exactly Is Subclinical Hyperthyroidism?
Subclinical hyperthyroidism means your thyroid is nudging just a little too hard-enough to suppress TSH (thyroid-stimulating hormone) below 0.45 mIU/L, but not enough to push free T4 or T3 out of the normal range. It’s not overt disease. It’s a quiet signal. And it’s more common than you think. In people over 75, up to 1 in 6 have it. Often, it’s found by accident during a checkup for something else.
The cause matters. Two main types exist: endogenous and exogenous. Endogenous means your own thyroid is overactive-usually from a toxic nodule or early Graves’ disease. Exogenous? That’s when you’re taking too much thyroid medication, often after being treated for hypothyroidism. The treatment approach changes depending on which one you have.
Why Your Heart Is the Real Concern
Forget the classic symptoms of hyperthyroidism. With subclinical cases, the biggest dangers aren’t felt-they’re measured. Your heart doesn’t wait for symptoms to start taking damage.
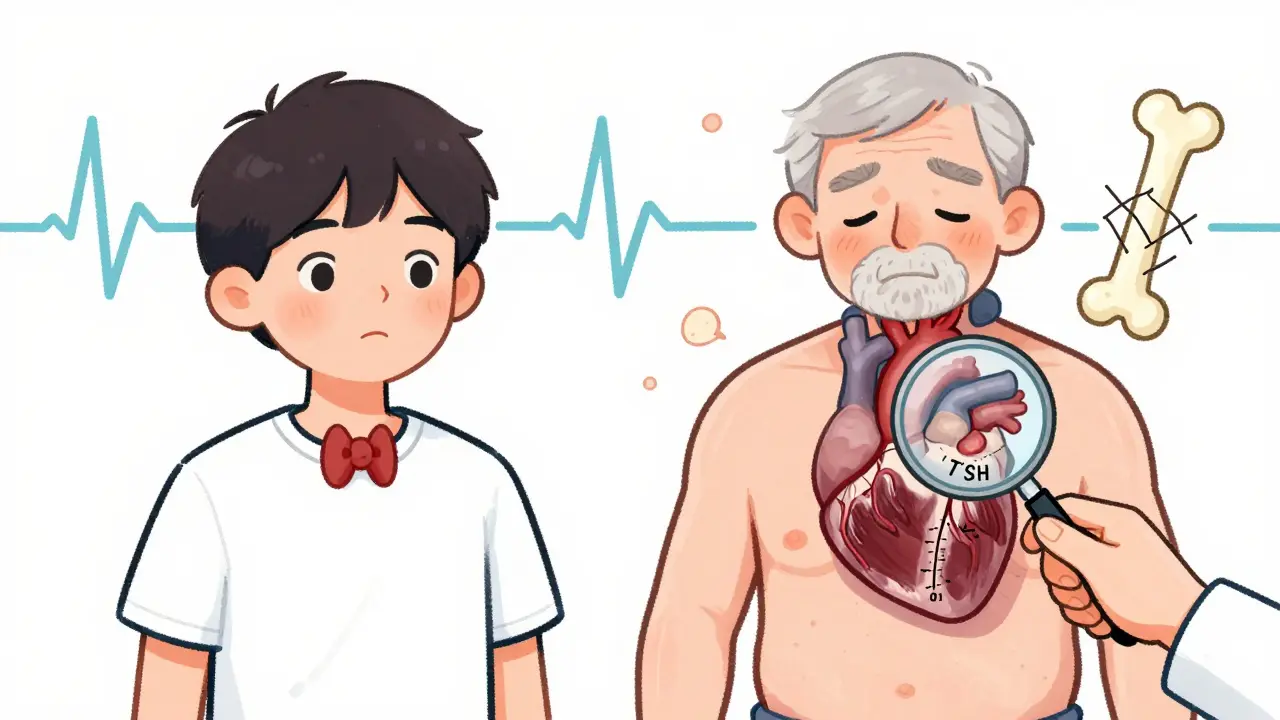
When TSH drops below 0.1 mIU/L, your risk of atrial fibrillation jumps. Studies show you’re more than twice as likely to develop this dangerous irregular heartbeat compared to someone with normal thyroid function. Even when TSH is just mildly low-between 0.1 and 0.44 mIU/L-you’re still 60% more likely to get it. Atrial fibrillation doesn’t just cause palpitations. It raises your stroke risk, weakens your heart over time, and can lead to heart failure.
And it’s not just rhythm. Your heart muscle thickens. The left ventricle gets stiffer. Diastolic function declines. Heart rate variability drops, meaning your body loses its ability to calm down after stress. All of this happens silently. You might feel fine, but your heart is working harder than it should.
One study followed 71 people with subclinical hyperthyroidism for years. Those with TSH under 0.1 had nearly five times the risk of heart failure. Another study of over 25,000 people found that those with the lowest TSH levels were almost twice as likely to develop heart failure over 10 years.
Bone Loss and Brain Fog: The Hidden Costs
It’s not just your heart. Your bones are also at risk. When TSH stays below 0.1 mIU/L long-term, bone mineral density drops. One study showed a 2.3 times higher risk of fractures-especially hip and spine fractures-in older adults. That’s not just a concern for osteoporosis. It’s a direct link to mobility loss and hospitalization.
Some research also suggests subtle cognitive changes. Elderly patients with persistent low TSH show small declines in executive function-planning, memory, and decision-making. It’s not dementia, but it’s enough to notice if you’re managing medications or finances on your own.
Quality of life? Usually fine in mild cases. But once heart symptoms creep in-fatigue, shortness of breath, dizziness-things change fast. That’s when the silent condition stops being silent.
Who Needs Treatment? It’s Not One-Size-Fits-All
Here’s the hard truth: not everyone with subclinical hyperthyroidism needs treatment. But some absolutely do. The decision isn’t based on the number alone-it’s based on your age, your heart, your bones, and your life.
If your TSH is below 0.1 mIU/L and you’re over 65? Treatment is strongly considered. Same if you have existing heart disease, high blood pressure, or osteoporosis. Even if you feel fine, the numbers tell a story your body can’t ignore.
For TSH between 0.1 and 0.44 mIU/L? Watch and wait-unless you have symptoms or other risk factors. If you’re young, healthy, and have no heart issues, you might never need treatment. But if you’re 70, have atrial fibrillation, and your TSH is 0.3? That’s a different story.
Doctors don’t treat the lab result. They treat the person.
Treatment Options: What Works and What Doesn’t
If treatment is needed, the goal isn’t to fix the thyroid-it’s to protect your heart and bones.
For patients with exogenous causes-meaning too much thyroid medication-the fix is simple: lower the dose. Many people don’t realize they’re on too much. A small reduction can bring TSH back into range without side effects.
For endogenous causes like toxic nodules, options are more involved. Radioactive iodine is often used to shrink the overactive tissue. Surgery is another option, especially if the nodule is large or suspicious. Both carry risks, including turning the condition into hypothyroidism-which comes with its own heart risks. That’s why doctors are cautious.
Beta-blockers like metoprolol or atenolol aren’t a cure, but they’re a bridge. They slow your heart rate, reduce palpitations, and can even help reverse some of the thickening in your heart muscle. Many patients feel better within weeks. But they don’t fix the root problem. They just buy time.

Monitoring: How Often Should You Get Checked?
If you’re not being treated, monitoring is non-negotiable. TSH can drift. Your risk changes over time.
- If your TSH is below 0.1 mIU/L: check every 3 to 6 months. Watch for rising heart rate, new irregular beats, or bone pain.
- If your TSH is between 0.1 and 0.44 mIU/L and you’re under 65 with no risk factors: annual testing is enough.
- If you’re over 65, even with mild suppression: every 6 to 12 months. Don’t skip it.
Don’t forget to track your heart health. An ECG every year, especially if you’re over 60, can catch atrial fibrillation early. A bone density scan every 2 years if you’re at risk for fractures.
The Big Debate: Treat or Wait?
There’s no global agreement. The European Thyroid Association says: treat everyone with TSH under 0.1. The American Thyroid Association says: it depends. Why? Because overtreatment can create new problems.
Turning subclinical hyperthyroidism into hypothyroidism isn’t harmless. It raises cholesterol, increases heart disease risk, and can cause fatigue and depression. Some older patients end up worse off after treatment.
That’s why experts like Dr. Kenneth Burman warn against treating mild cases without clear signs of harm. And why others, like Dr. Anne Cappola, argue that the heart risks are too high to wait.
Right now, the best advice is this: if you’re over 65 and your TSH is below 0.1, treat it. If you’re younger and healthy, monitor closely. If you have heart disease or osteoporosis-even with mild suppression-talk to your doctor about treatment.
What’s Next? Research Is Changing the Rules
Science is catching up. The DEPOSIT study, tracking 5,000 older adults across Europe, will finish in 2026. It’s the first large trial designed to answer whether treating subclinical hyperthyroidism actually reduces heart attacks and strokes.
Meanwhile, the THAMES trial at UCLA is testing whether early intervention improves heart outcomes in patients with TSH under 0.1. Early data suggests yes-but we need more.
For now, the message is clear: subclinical hyperthyroidism isn’t harmless. It’s a slow-burning fire in the heart. And if you’re over 65, or have other risk factors, it’s time to pay attention-even if you feel fine.






Joni O
January 18, 2026 AT 00:35My grandma had this and didn’t know it-just kept saying she was ‘tired all the time’ and ‘forgetful.’ Turned out her TSH was 0.08. They lowered her synthroid dose and she’s been walking her dog daily again. No drama, just quiet recovery.
Don’t ignore the quiet stuff.
It’s not ‘just a number.’
Jake Moore
January 18, 2026 AT 23:50As a primary care doc, I see this all the time. People freak out when their TSH is 0.3. Meanwhile, they’re 28, run marathons, and have no symptoms. We don’t treat lab values-we treat people. If your heart’s fine and you’re not old, chill. Monitor. Don’t panic.
But if you’re 72 with AFib? Yeah, let’s talk.
Dayanara Villafuerte
January 19, 2026 AT 15:02So… you’re telling me my ‘anxiety’ and ‘brain fog’ since 2021 was just my thyroid whispering? 😅
My endo finally lowered my levo dose last month. My heart stopped feeling like it was trying to escape my chest. Still waiting for my brain to catch up. 🤷♀️
Praseetha Pn
January 19, 2026 AT 19:05Oh, so now they’re blaming your heart problems on thyroid meds? Classic pharma distraction. Did you know the FDA approved synthetic thyroid hormones after a secret 1970s meeting with Monsanto? They want you dependent. Bone loss? Heart issues? That’s not the disease-that’s the side effect of the solution. Your doctor’s paid. You’re the product.
Go natural. Seaweed. Sunlight. Stop trusting labs.
christian Espinola
January 20, 2026 AT 10:41Another fear-mongering article written by someone who’s never met a patient. ‘Silent fire in the heart’? Dramatic. If you’re asymptomatic and under 65, you’re fine. The real epidemic is overmedicalization. People are getting treated for numbers, not symptoms. Next thing you know, we’ll be prescribing beta-blockers for ‘low-normal’ blood pressure. Pathetic.
Max Sinclair
January 21, 2026 AT 14:32I appreciate how this breaks it down without hype. My mom’s TSH was 0.28 at 71, had a tiny nodule, no symptoms. They monitored for 8 months, did an echo, a bone scan-turned out she was fine. No treatment needed. Just knowing the risk made her more proactive about walking and calcium. That’s the win.
Not every low TSH needs a fix. But every low TSH deserves awareness.
Wendy Claughton
January 21, 2026 AT 15:36I’ve been living with subclinical hyperthyroidism for 5 years now-TSH hovers between 0.2 and 0.3. I feel… fine? But I do get this weird flutter in my chest after coffee. So I cut out caffeine. I started doing yoga. I get an ECG every year. I don’t take meds. I don’t panic. I just… listen. My body’s whispering. I’m learning to hear it. 🌿
Not every problem needs a pill. Sometimes it just needs a pause.
Chuck Dickson
January 22, 2026 AT 23:06Hey, if you’re over 65 and your TSH is below 0.1, please-just talk to your doctor. I lost my uncle to a stroke because he ignored his ‘mild’ thyroid thing. Thought it was ‘just aging.’ It wasn’t. It was his heart screaming for help. You don’t have to be scared. But you do have to be smart.
Check your pulse. Get an ECG. Eat greens. Move your body. That’s not fear. That’s love for your future self. ❤️
Ryan Otto
January 24, 2026 AT 12:43Let’s be clear: the entire thyroid industry is a $40 billion scam built on the back of overtested, overmedicated elderly Americans. The American Thyroid Association is funded by pharmaceutical conglomerates. The DEPOSIT study? A placebo-controlled trial designed to validate pre-existing bias. The real risk? Being prescribed radioactive iodine at 70 and becoming a lifelong hypothyroid statistic. This isn’t medicine. It’s profit-driven pathology. Question everything.